Immuno-oncology is one of the most-watched medical research areas of the 21st century. Many cancer patients have experienced remarkable responses when treated with immunotherapy and there are currently almost 1000 immunotherapies in clinical development.
Immunotherapies harness a patient's own immune system to enable it to recognize and attack cancer cells. The immune system is very complex with multiple components; therapies can have an action on the components themselves, their mechanism of action or their communication pathways.
Consequently, there are many types of immunotherapy, including:
- Monoclonal antibodies and tumor-agnostic therapies
- Non-specific immunotherapies (interferons, interleukins)
- Oncolytic virus therapy
- Checkpoint inhibitors
- T-cell therapy
- Cancer vaccines
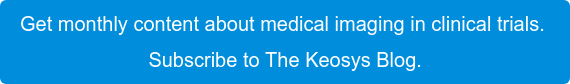
The latest immunotherapies to have been developed are based on:
- Checkpoint inhibitors. These block proteins that are used by tumors to evade the immune system. This enables the patient's own T cells to fight the cancer.
- Chimeric antigen receptor (CAR)-T cell therapy. This approach genetically modifies a patient’s T cells adding a code for a new surface protein that will target cancer cells.
Several of them already have regulatory approval, and many more are in clinical trials. The table below highlights approved drugs, together with their target and mechanism of action.
Challenges with Imaging Endpoints
Medical imaging is often used to monitor patient response to therapy in clinical trials. However, immunotherapies have a different mechanism of action from the traditional chemotherapies and conventional response evaluation criteria (RECIST 1.1) may underestimate the benefit of immunotherapy.
For example, when assessing imaging endpoints:
- The response of a tumor to immunotherapy is often delayed. This means that the immunotherapy can be mistaken as ineffective in the first couple months of monitoring.
- Before the tumors begin to shrink, they sometimes seem to increase in size for a couple of months because of the inflammation caused by the immune response. This is called 'pseudoprogression' or 'tumor flare'.
- Not all patients respond the same way. Some patients have striking responses, but others do not respond and some even experience severe side effects.
A specialist imaging CRO, that has a wealth of experience in medical imaging, can help smooth out these challenges. An imaging CRO will have expertise in the complex medical imaging technology, imaging protocols, state-of-the-art image acquisition and analysis, data management and quality control. This means they will ensure immunotherapy endpoints are assessed as efficiently as possible.
Immunotherapy-Specific Response Criteria
To face endpoint challenges, new response criteria have been developed, that aimed to better capture the response patterns observed with immunotherapies. Although there are differences between these criteria, all account for a potential delayed response and flare effect:
- Immune-related response criteria (irRC): No longer widely used.
- Immune-related RECIST (irRECIST): Together with RECIST 1.1, used in the majority of current immunotherapy clinical trials.
- Lymphoma response to immunomodulatory therapy criteria (LyRIC)
- Immune RECIST (iRECIST): Emerging criteria that aims to standardize and validate immune response criteria; acknowledges that only some patients will have pseudo-progression.
Traditional clinical trial endpoints — like overall survival and progression-free survival — may have limited ability limited to predict the long-term survival of patients treated with immunotherapies.
Immunological effects can linger for several months or even years. other endpoints, such as objective response rate and milestone survival (the survival probability at a given time point) have been proposed to account for this.
Because of the specificity of the interactions between a subject’s immune system and the cancer cells, imaging strategies using antibodies are used in subject selection and tumor monitoring. The goal is to maximize responsiveness while decreasing toxicity levels.
A Key Role for Radiologists
Immunotherapies have changed treatment strategies for cancer patients. The key role of radiologists in the care of these patients through staging/restaging exams necessitates specialized training. Radiologists must be able to understand the atypical tumor response, as well as the unique spectrum of immune-related adverse reactions, which may be first identified using CT or PET/CT scans. There is also an important role for medical imaging professional in the development of biomarkers, which will help bring immunotherapies to even more patients.