Historically, computed tomography (CT) has been the main imaging modality used to diagnose, treat, and monitor lymphoma. More recently, positron emission technology (PET) has been used to assess the metabolic rate of cancerous tissues by tracking the uptake of radiotracers such as 18-fluorodeoxyglucose (FDG).
The use of PET imaging means that lymphomas can now be detected and evaluated in more detail, using parameters other than simply size. This has become a significant advantage as imaging and treatment technology continue to advance.
In this post, we will talk about the role that modern imaging techniques play in diagnosing, treating, and monitoring lymphoma.
Historical Use of Imaging to Diagnose Lymphoma
The Cheson 1999 standardized response criteria were largely based on anatomic parameters but, as technology progressed, PET came into use to assess tumor metabolism. This was reflected in the updated Cheson 2007 criteria classified disease sites as either FDG-positive or FDG-negative.
It later became evident that a more nuanced scale was needed to evaluate FDG-avid lesions, which led to the development of the Deauville five-point scale. This compared the maximum FDG uptake at the initial disease site to two control sites (the mediastinum and the liver). This scale was incorporated into the Lugano 2014 recommendations, which are the most up-to-date recommendations for lymphoma evaluation, staging and response assessment.
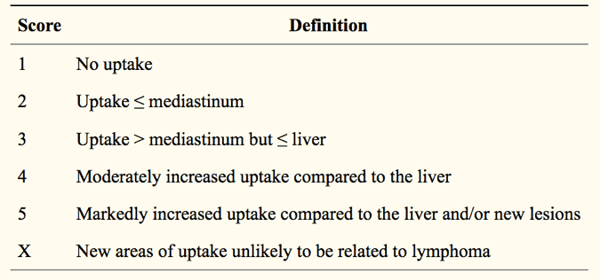 Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5541086/
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5541086/
The Current Role of Imaging in Lymphoma Evaluation and Treatment
Continuing advances in imaging technology mean that the approaches used to assess lymphoma progression are constantly evolving. For example, modern PET cameras are more sensitive than earlier versions and have a better signal-to-noise ratio, so they can detect smaller differences in FDG signals with more sensitivity.
Another important advance has been the development of hybrid PET/CT scanners, which generate images that integrate anatomical information with metabolic information. This means that disease sites can be staged more accurately; indeed, one systematic review found that ‘FDG-PET/CT fusion outperforms both CT alone and FDG-PET alone’ in accurately staging malignant lymphoma. Combining PET and CT can also help improve treatment targeting, for example by incorporating this imaging approach into radiation treatment planning.
However, FDG-PET/CT is not always the best choice for all lymphoma disease sites. For example, while FDG-PET can provide valuable clinical information if there is bone marrow involvement, biopsy or MR imaging are often indicated as well. In addition, ‘FDG uptake by gastrointestinal tract lymphoma is variable’, so alternative imaging techniques may also be recommended. MR imaging is also considered to be ‘the primary imaging modality for CNS evaluation in lymphoma’.
The stage of the lymphoma and its aggressiveness may also affect the utility of FDG-PET imaging. Importantly, as mentioned above, lymphomas can be FDG-positive or FDG-negative, depending on their rate of metabolism (and therefore progression), so lymphomas ‘with low or variable FDG uptake should still be staged with CT’.
Combining Imaging with Other Assessment Modalities
As imaging technology has advanced, other techniques for diagnosing and monitoring lymphoma have also continued to develop. Many of these new techniques can be combined with imaging to provide valuable information about disease progression and predict outcomes. One study explored the correlation between tumor proliferation in patients with untreated mantle cell lymphoma as assessed by FDG-PET/CT, gene expression profiling, detecting actively dividing cells with an MIB1 antibody, and evaluating serum levels of lactic acid dehydrogenase.
This study showed that ‘low and intermediate SUV values do not reliably correlate with tumor proliferation’ as assessed by other methods, unlike high SUV values, suggesting that combining imaging with other approaches can provide important clinical information.
Imaging can also be combined with more well-established gene expression analysis techniques. A recent study of diffuse large B cell lymphoma that analyzed MYC rearrangements in patients who underwent FDG-PET/CT interim imaging after receiving chemotherapy. This study found that combining these two approaches ‘might provide increased prognostic value for DLBCL’.
In addition to these well-characterized evaluation methods, new biomarkers have come into use. Many of these biomarkers are based on radiomics, which is the use of imaging data to investigate image-based features and evaluated their association with disease stage and progression. Radiomics biomarkers include more traditional tumor features such as SUV, contrast, and homogeneity, as well as newer approaches to evaluating tumor progression, such as total lesion glycolysis and metabolic tumor volume (MTV). For example, MTV can be used to evaluate lymphoma progression by measuring the volume of individual FDG-positive lesions; and the volumes of all of the lesions can be added together to determine the total MTV throughout the body.
Looking to the Future: New Imaging Developments and Guidelines
In addition to providing new ways of assessing and treating lymphoma, recent advances have created some challenges to the use of imaging in lymphoma management. One area where this is particularly true is in patients receiving immunotherapy for lymphoma treatment. In patients receiving passive immunotherapy, which involves the infusion of antibodies targeting tumor-specific antigens, the response generally follows the typical progression seen with chemotherapy.
Due to these differences in treatment response, new guidelines have been suggested for evaluating patient response to immunotherapy, including immune-related response criteria (irRC), immune-related RECIST (irRECIST), and immune RECIST (iRECIST). Key aspects of these new guidelines include performing multiple follow-up imaging assessments after completion of treatment to detect delayed responses and changes in the overall tumor burden.
Finally, imaging also plays an important role in monitoring patient safety during immunotherapy, as ‘immune-related adverse events may be detected earlier with FDG PET/CT and can precede clinical symptoms, allowing early therapeutic interventions’.