Positron emission tomography (PET) imaging is widely used to assess tumoral activity, blood flow, cells proliferation or apoptosis in the body. PET scanners detect the radiation given off by a tracer, and analysis of areas where the radiotracer builds up makes it possible to identify potential abnormalities. For example, the common radiotracer fluorodeoxyglucose (18F-FDG) can identify cancerous cells because of their increased rate of glucose metabolism.
Other PET tracers, such as those specific for tau proteins (Tau-PET, e.g. 18F-AV1451 PET) found in neurological disorders, and metallic tracers like 68Ga-PET (which are useful to image ligand–peptide receptor interactions in certain cancer types) are examples of the wide range of PET tracers available for clinical research. In this blog post, we look at examples that highlight the power of PET imaging in clinical research, and note some key considerations for using PET. Another of our blog posts on PET can be found here.
Why Use PET Imaging in Your Clinical Trial
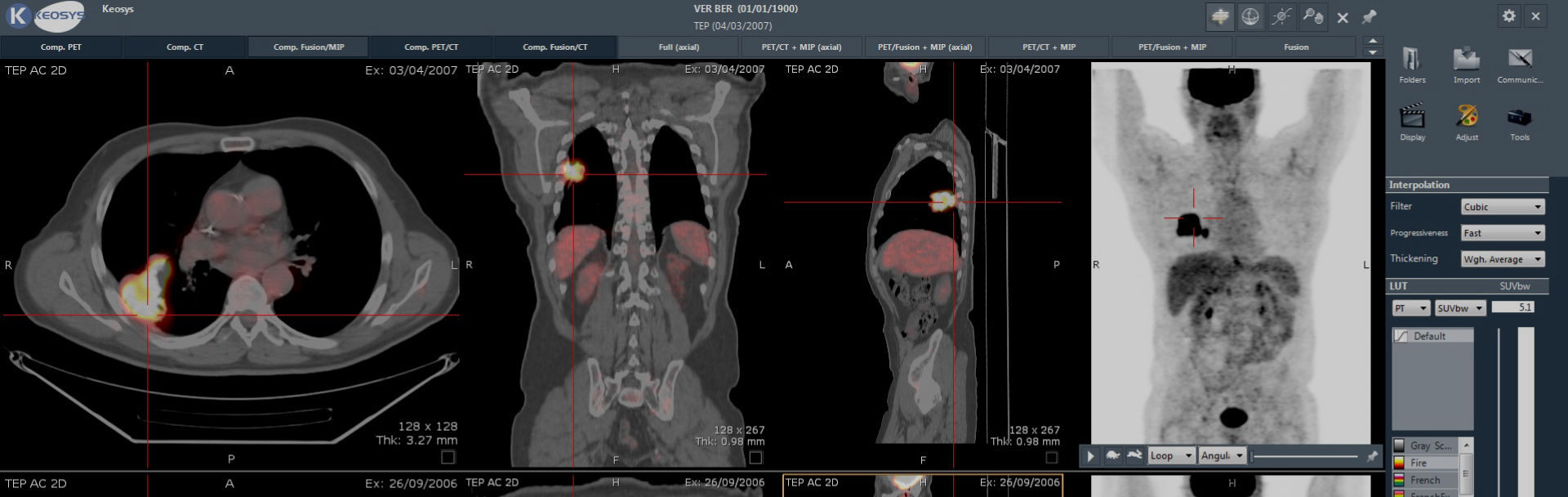
A PET scan shows how a tissue works by providing functional imaging. However, it can be difficult to pinpoint the exact body location of this activity. The combination of PET with the anatomical imaging of CT (PET/CT) to assess tissue size and shape, makes a powerful tool for use in clinical trials.
PET/CT imaging can identify patients who might benefit from treatment (and equally important from those who won’t) and can aid the fine-tuning of efficacy monitoring. One approach uses the molecular expression pattern of molecules (e.g., receptors, transporters, and enzymes) overexpressed on cancer cells that can be targeted with a specific target ligand (e.g., peptide analogs or antibodies). As we'll highlight in more detail later, such target-mediated imaging is used in patients with neuroendocrine tumors.
Examples of PET Imaging in Clinical Trials
In some areas, such as Hodgkin’s and non-Hodgkin’s lymphomas, PET scans are part of the standard of care. They are routinely used for staging and treatment monitoring, and can predict progression-free survival and patient outcome in certain sub-indications, such as follicular lymphoma.
Theragnostic and Peptide Receptor Radiotherapy
In other areas, the involvement of PET/CT is more novel. Theragnostic combines a specific targeted therapy based on a specific targeted diagnostic test. An example is Lutathera, a treatment for neuroendocrine tumors, together with the diagnostic Netspot. This theragnostic platform makes use of a molecule that binds to peptide receptors over expressed in neuroendocrine tumors. A somatostatin analog is either radiolabeled with 68Ga to produce the diagnostic, or with 177Lu to produce Lutathera. In this way, diagnosis of the disease can be followed by treatment and efficacy assessment using the same molecular targeting compound with PET/CT.
Alzheimer’s Disease
PET/CT has a key role in Alzheimer’s disease (AD), where an unresolved challenge is to diagnosis the disorder before symptoms become apparent. AD is characterized by amyloid-β (Aβ) plaques and neurofibrillary tangles made up of aggregated tau proteins. Aβ-PET imaging is FDA-approved to diagnose AD and distinguish from cognitive impairment, and is used in clinical trials of anti-Aβ therapies both for patient recruitment and as an outcome measure. Of note, Tau is probably a better predictor of cognitive performance than Aβ deposition. This indicates that Tau imaging may be particularly useful for monitoring changes in brain function that are responsible for early symptoms in AD.
Considerations for Using PET in Clinical Trials
Quality data is key for PET/CT to reach its full potential in clinical studies. To achieve this, there are several considerations that should be considered.
- Standardization of imaging procedures: The uptake time of the tracer compound must be standardized (standardized uptake value; SUV), as this parameter is used to distinguish between 'normal' and 'abnormal' levels of uptake. As such it is used for patient inclusion/exclusion, response monitoring and as an imaging biomarker.
- Mandatory collaboration: In a multi-center trial, PET scanners will have different manufacturers and technical specifications and will be used according to local practices. Calibration of PET scanners across sites is mandatory to ensure comparable quantification.
- Adherence to standards: These include QIBA profiles, which provide technical performance standards emphasizing the importance of reproducibility and repeatability and the UPICT Concept, which develops consistent imaging protocols across disease states, anatomic sites and imaging modalities.
- Precise reading criteria: How images are interpreted and how potential sources of imaging bias and variability are controlled should be recorded in a charter specific for that clinical trial.
This blog post has only touched upon the wide potential of PET/CT imaging in clinical studies, but it has highlighted key roles such as monitoring treatment efficacy in cancer. In addition, it's hoped that PET/CT imaging will be able to be used to identify pre-symptomatic disease in AD, and importantly, distinguish AD from mild cognitive impairment. There are many disease- pathway- and physiology-specific tracers available to aid clinical research, and new tracers will undoubtedly be identified. Added to this, the development of new PET technologies — such as total body PET and increases in PET sensitivity — will open up even more opportunities for PET/CT.