Imaging biomarkers are often pivotal components of a clinical trial, from patient selection to serving as surrogate endpoints or monitoring safety. However, developing a relevant, accurate and cost-effective imaging biomarker is frequently a formidable challenge.
Using various disease-specific examples, this post discusses some of the issues of imaging biomarker development.
Mini Overview
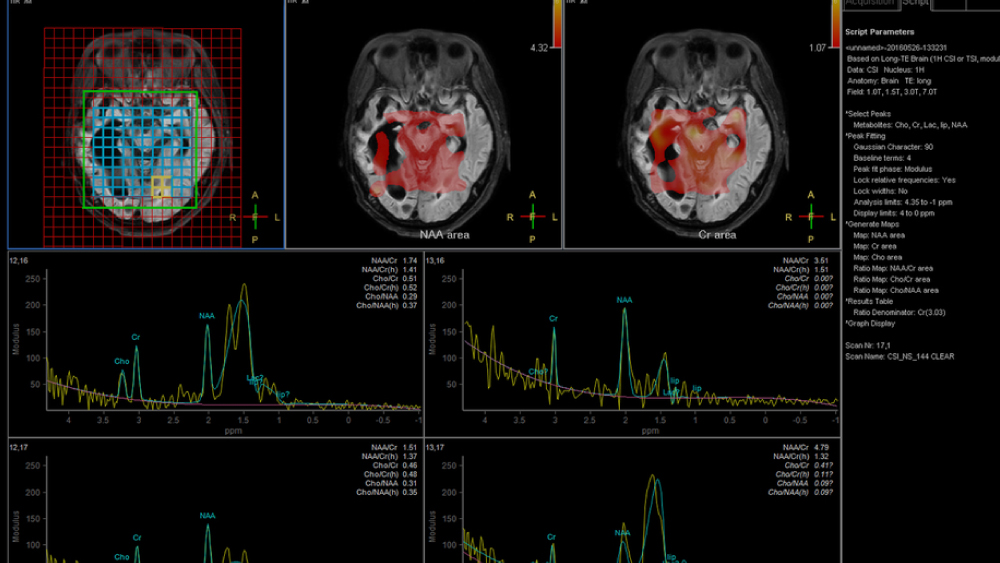
Imaging biomarkers are usually obtained from PET, MRI and CT scans and comprise measurements of structural and metabolic features of the body. For example, measurements of a tumor’s diameter/volume or different areas of the brain (structural) or glucose uptake (metabolic) over time are used to assess disease progression and response to treatment in conditions such as cancer and Alzheimer’s.
Imaging biomarkers are also helping to streamline drug development and facilitating the realization of ‘personalization’ medicine. Biomarkers (qualitative or quantitative) can serve as predictive, prognostic, mechanistic or surrogate markers (see Box 1 for definitions) depending on what they are measuring. However, a newly developed imaging biomarker must also be validated and standardized for it to be effective (see Box 1 for definitions).
Below, we provide a few examples of imaging biomarker development for specific indications.
Alzheimer’s disease is underpinned by a complex pathophysiology. This complexity is hampering the development of disease-modifying drugs for this prevalent neurodegenerative disorder. Particularly challenging is the fact that changes in the brain structure occur decades before clinical symptoms become apparent. Consequently, many diverse drug targets are being pursued, as are many biomarkers.
Biomarkers are proving their value in distinguishing between different forms of dementia and tracking disease progression. For example, structural MRI estimates of tissue damage or loss in brain regions such as the hippocampus and entorhinal cortex are predictive of progression of mild cognitive impairment to Alzheimer’s. Moreover, whole-brain and hippocampal atrophy rates are sensitive markers of progression of neurodegeneration, and are increasingly used as surrogate endpoints in clinical trials.
As noted above, effective biomarkers must also be standardized and validated. Fortunately, groups such as the Alzheimer’s disease Neuroimaging Initiative (ADNI) are successfully addressing these challenges. For example, the MRI core of the initiative has created standardized acquisition protocols and quality control methods. Data published by the ADNI are open to researchers to develop their own models and hypotheses for testing. For example, one study used ADNI data from multiple modalities (imaging and other biological markers) and machine learning techniques to identify 12 distinct Alzheimer’s disease states. The authors hope that such models will help to more accurately match patients with therapies targeting specific aspects of the disease.
Patient Staging in Prostate Cancer
Among the modalities used to assess prostate cancer, PET imaging is proving superior to conventional imaging (e.g., CT, prostate-specific membrane antigen (PSMA) imaging and bone scan) in the staging of extraprostatic disease. Accurate staging of disease is vital to enable accurate treatment plans.
Among the PET tracers developed, 11C-choline and 18F-choline have influenced prostate cancer imaging, particularly in biochemical relapse. Choline is a marker of cell membrane synthesis and prostate cancer cells show altered levels of choline. The utility of this tracer led to the US Food and Drug Administration to approve 11C-choline for identifying patients with recurrent disease.
Meanwhile, future promising PET imaging biomarkers to look out for include those that that have theranostic capabilities, such as 18F-rhPSMA. In addition to its utility in patient staging in prostate cancer, these radiohybrid tracers can be labelled with radioisotopes such as 177lutetium or 225actinium for therapeutic use.
Disease Progression in Breast Cancer, Lung Cancer and Melanoma
The exponential growth in our understanding of cancer at the genetic and molecular level is fueling efforts to develop imaging biomarkers to reflect these subtleties. For breast cancer, lung cancer and melanoma, the development of imaging biomarkers must also keep pace with the type of therapeutics being developed.
For example, cytotoxic chemotherapy, which causes cell death and decreases tumor size, is ably monitored using RECIST via CT scans. Conversely, molecularly targeted therapies tend to inhibit tumor growth instead of causing regression. Consequently, detecting changes in the vascular microenvironment (e.g., via FDG-PET scans or diffusion-weighted MRI) of the tumor becomes more important than assessing changes in tumor size. Bearing these factors in mind is important when developing imaging biomarkers for different diseases and therapeutics.
Future Trends
The development of imaging biomarkers is subject to intense efforts, and several pathways have been proposed to ensure rigor. For example, the “Imaging biomarker roadmap for cancer studies” and the “Strategic roadmap for an early diagnosis of Alzheimer's disease based on biomarkers” are among many initiatives (see Box 2) setting out detailed guidelines to help propel the field forward. From a regulatory perspective, the US Food and Drug Administration a comprehensive program of support and dialog to promote the development of qualified biomarkers.
Meanwhile, radiomics in particular is an area of great promise. This field harnesses advances in technological capability and computing power to enable high-throughput quantitative image analyses. And, similar to imaging biomarker development, an initiative has already sprung up, proposing guidelines and definitions to help ensure standardization.
Mechanistic – a biomarker that aims to show that the drug has an anatomical, functional or biological effect on the target.
Predictive – a biomarker that aims to forecast disease course, treatment response or risk of toxicity.
Prognostic – a biomarker that aims to forecast survival/clinical benefit.
Qualitative – a biomarker that requires expert interpretation.
Quantitative – a biomarker that is based on mathematical definitions.
Surrogate endpoint – a biomarker intended to substitute for a clinical endpoint.
Testing imaging biomarkers
Standardization - the biomarker must exhibit reproducibility across different centers and machines with respect to acquisition parameters for imaging and the post-processing methods.
Validation – the biomarker must exhibit sensitivity, specificity, precision and reproducibility. Changes in biomarker values should be correlated to the biological effect and clinical endpoints (qualified). Validation requirements are usually much higher for surrogate endpoints than for mechanistic biomarkers.
Several public-private partnerships aim to address challenges in the development and adoption of imaging biomarkers. A selection is provided below.
QuIC-ConCePT – an Innovative Medicines Initiative-funded project designed to qualify imaging biomarkers of tumor cell proliferation, apoptosis and necrosis.
National Cancer Institute’s Cancer Imaging Program – fosters advances in in vivo medical imaging sciences to gain greater understanding of the pathways of cancer biology.
Society of Nuclear Medicine and Molecular Imaging’s Clinical Trials Network – aims to facilitate the effective use of molecular imaging radiopharmaceuticals in clinical trials through standardization, coordination, and education.
Radiological Society of North America’s QIBA – aims to advance quantitative imaging and the use of imaging biomarkers in clinical trials and clinical practice.